Aiming to provide availability, accessibility and affordability for all
In recent years, you may have heard about Aspen Valley Hospital’s efforts to promote population health, to bring more primary care providers to the community and to work toward achieving the Institute for Healthcare Improvement’s Quadruple Aim. These different initiatives may seem abstract, but they’re part of a united goal to transform the traditional healthcare model and ensure everyone has access to the right care at the right time in the right place for the right price.
Such a goal is as daunting and daring as it is necessary to the health of our community. And to achieve it, AVH has changed the way that it does business and joined forces with an array of other stakeholders in Pitkin, Garfield and Eagle counties to create the nonprofit Valley Health Alliance (VHA).

TEAM OF ‘RIVALS’
At first glance, it may be surprising to think of so many different kinds of organizations working together. After all, hospitals typically compete with each other for the best staff and technology; physicians often battle insurers for higher reimbursements; and employers and employees lament ever-increasing health plan costs.
In the Roaring Fork Valley, however, the picture is quite different. Among various stakeholders, there’s a growing awareness that cooperation makes sense for everyone.
“If we learned anything from the COVID-19 pandemic, it’s that partnerships are powerful tools for leveraging limited local resources for maximum effect,” said Dave Ressler, CEO of AVH. “Here in the mountains, we operate in a low-volume environment with associated inefficiencies, despite needing high-level capabilities to meet the needs of our community.”
That’s where innovative approaches, such as cooperative relationships among “rival” hospitals, become crucial. Although already underway, such cooperation got a significant boost from the public health crisis.
“During COVID-19, hospitals had a strong incentive to work together and communicate about available resources and capacity,” said Chris McDowell, Executive Director of the VHA. “You saw the entire medical system cooperate to be more effective and efficient. AVH, Valley View Hospital [in Glenwood Springs] and St. Mary’s Hospital [in Grand Junction] came together to communicate and share resources for the good of the community.”
CARING IS SHARING
Among the most high-impact examples of this cooperation in action is the coordination of medical specialties across the region. Today, AVH shares oncology, cardiology, urology, gastroenterology and breast surgery services with Valley View and has also partnered with Vail Health and The Steadman Clinic to provide orthopaedic care.
“AVH and its peer institutions have a common bond of being community-owned and -focused,” Ressler said. “We recognize that we can better serve our communities by working together to avoid redundancy of services and share high-cost specialties.”
McDowell, too, is heartened to see hospitals working together to address the special challenges of a rural community. “These hospitals are pooling resources and breaking down siloes,” he said. “If we work together in this way for the good of all, then we can better meet the healthcare needs of the community.”
The VHA has been instrumental in uniting the interests of hospitals as well as employers, insurers and other vested parties. About a decade ago, AVH began working with several large, self-insured employers — including Aspen Skiing Co., the City of Aspen, and Pitkin County — to bend the curve of their employee health costs. Alarmed by double-digit annual increases, they joined in an effort to drive changes that would ensure the long-term availability, accessibility and affordability of healthcare.
Those conversations led to the VHA’s formation in 2014 with an initial focus on employee wellness, engagement and disease prevention. By most measures, the work was successful, except that it didn’t do enough to rein in costs. McDowell was hired in 2017 to bring a sharper focus to primary care as a way to advance the Quadruple Aim:
- Improve the quality of care and patient experiences;
- Enhance physician engagement;
- Elevate population health status and wellness; and
- Reduce costs.
PRIMARY CONSIDERATIONS
Success in these areas hinges on primary care providers as guides. The primary care providers’ role is to understand patients’ health history, manage risks, provide preventive services, treat chronic conditions and coordinate specialty care. It is the primary care provider’s position as the hub of healthcare that attracted Kelly Locke, MD.
“There is never a dull day in the office,” said Dr. Locke, Medical Director of Aspen Valley Primary Care. “The patient who presents with a shoulder complaint often has concerns about chest pain, toenail fungus and work stress — all in the same visit. As a primary care physician, I evaluate all of these problems and put the patient on a path to healing.”
Dr. Locke’s medical expertise is also proving useful in his role as a member of the VHA Board of Directors and its Clinical Advisory Board. “With my knowledge of the day-to-day life of a physician, I can help guide ideas that may impact how a clinic is managed and try to avoid ideas that might have a negative impact on patient care and the running of a busy practice.”
Primary care providers are also aligned with population health: the concept of managing the health of not only individual patients but also the wider community. For example, a person who suffers from chronic back pain may start missing work, which leads to a cascading series of complications: job loss, housing and food insecurity, mental health issues and more. “It’s all interconnected,” Dr. Locke said. “Population health includes direct medical services and factors that aren’t strictly medical but can affect individuals, their families and the overall population.”
Primary care providers also play an outsized role in managing healthcare costs. McDowell cited data showing that in 2018, about 250 people in VHA member organizations visited an emergency room for non-emergency upper respiratory illnesses. That emergency room care cost about $500,000 more than if those individuals had sought care from a primary care provider.
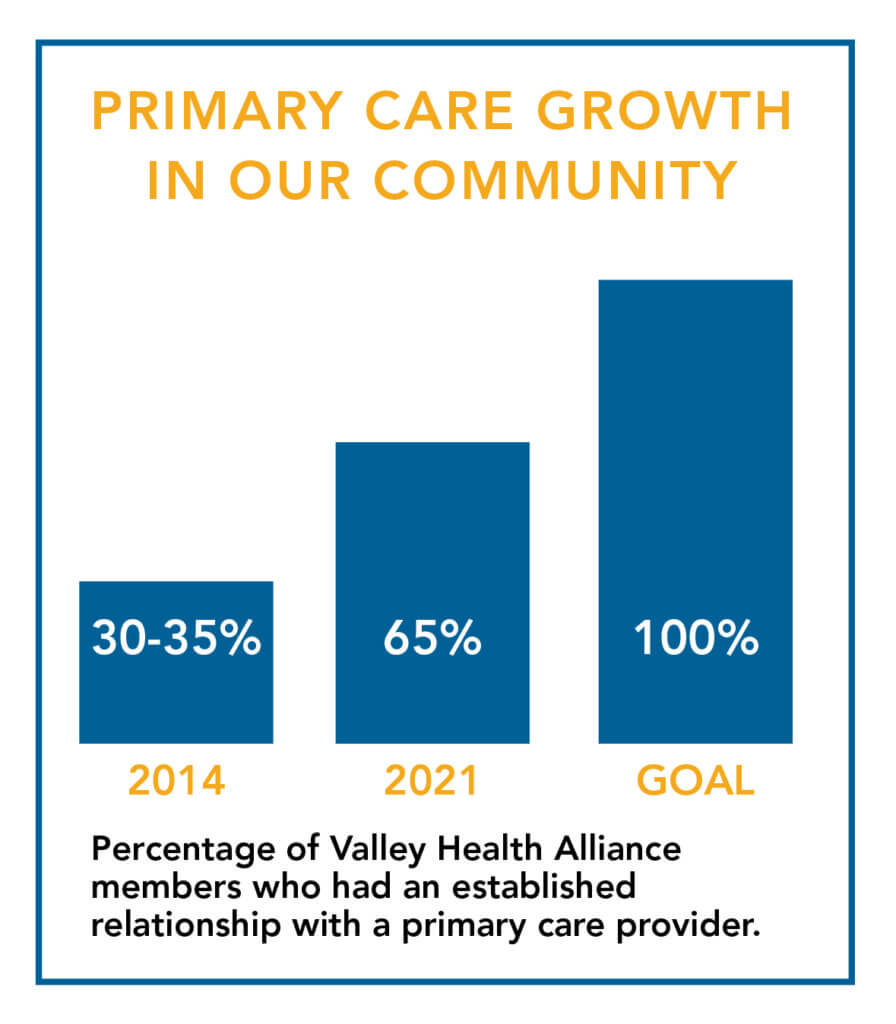
When the VHA was founded in 2014, only 30-35 percent of its members had an established relationship with a primary care provider. As of early 2021, the number had about doubled to nearly 65 percent. That’s good progress, but McDowell believes getting close to 100 percent will be an essential measure for long-term success. And this is why the Hospital is focused on building its primary care practice with providers who can address a wide range of non-urgent medical care for patients.
MONEY MATTERS
Healthcare is a multi-layered ecosystem, and cost is an important factor in many of the initiatives that VHA partners undertake. As Ressler said, “Quality healthcare should be accessible and affordable to all Americans, and in particular the members of our community. For most people, that means the cost of both healthcare services and health insurance.”

An important safeguard, health insurance still may have prohibitively expensive deductibles, copays and other out-of-pocket costs. On this front, VHA partner organizations celebrated a recent win with the introduction of new insurance options by Rocky Mountain Health Plans, part of UnitedHealthcare. Rocky Mountain Health Plans now compete with Anthem Blue Cross Blue Shield, which had long been the only insurer in the local market. The competition has been credited with lowering member premiums in the region by up to 15 percent.
Controlling costs is just one way the healthcare system is working more effectively in the Roaring Fork Valley. Access is another area that has received deserved attention. During COVID-19, when many patients and providers were forced to defer certain types of care, telemedicine was able to keep communication channels open.
“During the pandemic, telemedicine became an important tool that allows patients and providers to connect without having the patient travel to the office,” said Elaine Gerson, AVH Chief Operating Officer and General Counsel. “Going forward, this approach is certainly appropriate for follow-up visits, where a hands-on examination may not be necessary.”
Telemedicine is the kind of innovative approach that will help AVH and other community organizations “continue to move toward a value-based program for care,” Gerson said. “Our strategic plan has a focused effort on innovation, which includes continued work on delivery of care in a transformational way.”
TIME PASSAGES
Change rarely happens quickly, but its advance can be steady — a dynamic McDowell likens to eating an elephant one bite at a time.
The value-based approach to healthcare stems from federal legislation passed more than a decade ago: the Affordable Care Act of 2010. One of its main tenets is incentivizing physicians based on how effectively they manage their patients’ care rather than on how many patients they treat.
This model encourages everyone to “pull on the same rope,” McDowell said. “It’s a win for communities, employers, employees, providers and insurers. That is the essence of what we’re trying to accomplish.”
Ressler agrees but cautions that the task is inherently challenging. “Transformation of any kind is hard work, particularly in a complex system that has been decades in the making,” he said. “But it is a mandate for us to undertake the work ourselves. Our community has what it takes to be successful, and we’ll all be a part of the solution of achieving affordable and accessible healthcare — together.”
“Our community has what it takes to be successful, and we’ll all be a part of the solution of achieving affordable and accessible healthcare — together.”
— Dave Ressler, CEO of AVH
NEW APPROACH ENHANCES AVH’S MISSION OF ‘EXCELLENCE, COMPASSION AND TRUST’
As it works to transform healthcare in our community, Aspen Valley Hospital is not veering away from its mission — the hospital is embracing it more closely than ever before.
“We’re moving away from a volume-based system and toward better management of the patient’s health,” said Elaine Gerson, Chief Operating Officer and General Counsel at AVH. “Therefore, we’re doing exactly what our mission states: delivering extraordinary care in an environment of excellence, compassion and trust.”
For patients, transformation takes on many forms:
- AVH’s enthusiastic expansion of telemedicine as an important tool to connect with patients, especially during the COVID-19 pandemic.
- A greater emphasis on primary care and its teambased focus, with clinics bringing in care coordinators, behavioral health specialists, dietitians, clinical pharmacists and others to support patients.
- The addition of a physician assistant to Aspen Valley Primary Care to facilitate access to care for patients who may not need to see a physician.
- The addition of a pediatrician to the primary care services, complementing the practice’s family medicine and internal medicine physician providers.
Gerson noted that some other transformational changes might be less obvious to patients. “One of our goals was to increase access by establishing primary care locations in both Aspen and Basalt,” she said. “These types of strategic decisions not only provide better medical care today but are also designed to accommodate future demand for primary care services and providers.”

